
Dental Implant
Most of the people want to replace their missing tooth by Dental Implants. But due to lack of knowledge and huge cost, they are damaging their healthy natural tooth by trimming it and placing bridge. Here in DENTA SMILE we offer advanced type of dental implants for a common man at affordable price
A dental implant is actually a replacement for the root or roots of a tooth. Like tooth roots, dental implants are secured in the jawbone and are not visible once surgically placed. They are used to secure crowns (the parts of teeth seen in the mouth), bridgework or dentures by a variety of means. They are made of titanium, which is lightweight, strong and biocompatible, which means that it is not rejected by the body. Titanium and titanium alloys are the most widely used metals in both dental and other bone implants, such as orthopedic joint replacements. Dental implants have the highest success rate of any implanted surgical device
The basis for dental implants was a biologic process called osseointegration where materials, such as titanium, form an intimate bond to bone. The implant fixture is first placed, so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic (a tooth, bridge or denture) is attached to the implant or an abutment is placed which will hold a dental prosthetic. It took more time to get a fixed teeth. This concept have changed now a days. Now a days surgeons use cortical bone as primary stability area and place implants in cortical bone, i.e., for upper jaw we use Nasal Floor, Nasomaxillary buttress, Sinus floor, Pterigoid process And Zygomatic bone. And for lower jaw we use Base of the mandible for front tooth and Lingual or Buccal cortical bone for back tooth..
The dental implant team consists of an ORAL AND MAXILLOFACIAL SURGEON to place the implant, PROSTHODONTIST to plan and place the tooth restoration, PERIODONTIST to maintain healthy gum and bone around the implant or a general dentist with advanced training in implantology and a dental laboratory technician who fabricates them..
Single Tooth Replacement
Fixed Multiple Tooth Replacement
Removable Implant-Supported Tooth Replacement
Natural teeth and dental implants may look the same, feel the same, and even function in a similar way, but they are very different. The most important differences are in the way they attach to the surrounding bone, their response to dental disease, their maintenance, and repair. Teeth attach to the surrounding bone by a periodontal ligament (“peri” – around; “dont” – tooth) made up of collagen fibers that join into the tooth on one side and bone on the other. Dental implants fuse directly to the bone. The gum tissues also attach to the root of a tooth with collagen fibers as described above. However, gum tissues can only stick to the surface of dental implants. Teeth are susceptible to dental decay as well as the need for root canal therapy; dental implants are metal and do not decay or need root canal. Teeth may also be susceptible to periodontal (gum) disease, while dental implants may be susceptible to peri-implantitis, an inflammatory response to bacterial biofilm of the tissues surrounding the implant, which can result in disintegration of the bone to the implant.
- Basal implants (Immediate placement and loading implants)
- crestal implants(delayed placement and loading implants)
Basal or Immediate Placement Implants:
The term “Basal Implant”was invented in 1998. It reflects the idea and principle that the implant distribute load in basal bone. These areas are stable and the bone in this area does not resorb. The bone used for this implants, which remains as it is for several years. They are advanced implant system which utilizes the basal – cortical portion of the jaw bones for retention and stability of the dental implants. Basal implants are also known as Cortical Implants..
The surgical procedures are so simple that they are usually performed in the office with local anesthesia. First we have to extract the tooth which is damaged. As soon as extraction, the tooth socket is cleaned and drills are placed and basal implants are placed. If there is no tooth to be extracted then the implant procedure will be like a key hole surgery. We don’t have to reflect the flap. The procedure will be flapless and time consuming will be less. Same day impressions are taken and send to dental laboratory where the crowns are crafted. And crown is fixed on 3 rd day. Which allows you to be in normal life, just in 3 days. Basal implantology avoids second sitting for surgery.
Conventional implants are a tried and true type of implant that is performed in three sittings of treatment over 9-12 months. This type of implants are performed less frequently in most modern dental clinics, as the amount of time needed to complete treatment is the more. The first two sittings require about 3-5 days each, and the last require about a full week..
First, extraction of the tooth is performed and the gums/bone are allowed to heal before the implant is placed. Usually this takes about 2-6 months before the implants can be placed. Sometimes, artificial powdered bone material is placed into the empty extraction site to ensure there is enough bone to support the implant. This is called a minor bone graft or a socket graft. If the tooth was knocked out, or is already missing, you still need to wait 2-6 months from the time it was lost to have implants placed. Extractions, and socket grafts if required are typically done in one appointment. After the bone and gums heal, the extraction site is reopened and the dental implant can be placed. The implant is screwed into the jawbone itself and the gums are then sealed over the implant. Your jawbone will actually grow around the implant in a process called osseointegration and this needs to occur before the abutment and permanent crown is fitted. Usually it takes about 3-6 months for the implant to osseointegrate with your jawbone before it is stable enough to support the abutment and crown. Implants can be placed in just one appointment, but follow ups for suture removal, check-ups, etc. are required.After the implants are stable, you would return to have the abutment and crown fitted. During this visit, the gums are opened up, the abutments are attached to the implants, and then impressions are taken of the abutments and surrounding teeth in order to send off the dental laboratory where the crowns are crafted. It is important that good impression are taken so that when the crowns are fitted, they fit properly, align and match the bite of your other teeth, and have a proper minimal margin at the gumline for best appearance. It takes a few days for the lab to make the crowns, and the whole process usually takes about a week..

Immediate loading - Teeth loaded within 3 days of implant surgery
Single piece implantology- minimizes failure of implants due to interface problems between the connections which exist in conventional two and three piece implants
Basal bone support- most of these implants take support from the basal bone which are a lot more resistant to resorption, very much unlike the conventional implants which mostly take support from the crestal bone. Basal cortical bone also has a much faster and stable repairing capacity
Minimally invasive - in most edentulous situations, the single piece screw type implants can be inserted in a minimally invasive fashion – often flapless and involving minimum bone cutting. The implants are self tapping and condense bone around the implant during insertion. Being minimally invasive, they are also associated with minimum post operative edema and healing at the procedure sites are rapid and often non-eventful.
Unfavorable bone situations- Avoidance of bone augmentation / grafting, sinus lifts and nerve trans-positioning – These implants are unique in that they utilize the available bone in the best possible manner to avoid bone augmentation procedures. With conventional implants, the available bone is modified to suit the implants. With the basal implants, implants are selected or adapted to suit the available bone – with respect to quality and quantity. In the case of atrophied mandible, implants can be placed transversely (mainly the BOI implants are used here) above the mandibular canal taking the horizontal bone support or bicortical implants can be placed bypassing the mandibular nerve, engaging the lower cortical border of the mandible. Thus, bone augmentation / grafting procedures and complex procedures such as inferior alveolar nerve transpositioning are almost completely eliminated. In the case of atrophied maxilla with an unfavorable maxillary sinus situation for implants, the sinus is bypassed with the basal implants, taking support from the bone anterior and posterior to the maxillary sinus (tubero-pterygoid implants), thereby eliminating the need for bone augmentation and sinus lifts, almost completely.
Basal implants work extremely well in patients with acute destructive periodontitis- where the mobile teeth have little or no bone support at all by facilitating implant placement and immediate loading soon after extractions.
Peri-implantitis incidence -Peri-implantitis is the single most common cause for failure of conventional implants. Judicious use of basal implants eliminates the threat of peri-implantitis by almost 98%.
Revolutionary designs and features-of the basal implants help the implantologist in treating a wide variety of cases which cannot be attempted with the conventional two / three – piece crestal implants.
Medically compromised situations – Basal implants work fine in controlled diabetics, in smokers and in patients who have little or no bone for conventional implants. Thus, Basal implants offer a unique opportunity to the implantologist to treat cases which cannot be treated with the conventional implant system

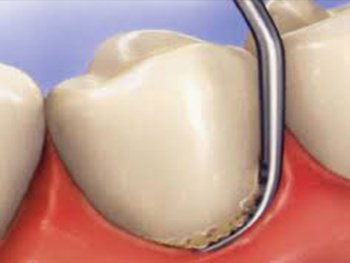
Scaling or professional cleaning is a conventional periodontal therapy, non-surgical periodontal therapy, or deep cleaning of tooth by removing or eliminating the causative agents such as dental plaque and calculus , which cause inflammation, thus helping to establish a periodontium(Gum) that is free of disease. It can also be done as prophylaxis which means “to prevent ”. It helps us to prevent gum (periodontal) disease..
Plaque is a soft yellow-grayish substance that adheres to the tooth surfaces including removable and fixed restorations. It is an organised bio-film that is primarily composed of bacteria in a matrix of glycoproteins and extracellular polysaccharides. This matrix makes it impossible to remove the plaque by rinsing or using sprays. Materia alba is similar to plaque but it lacks the organized structure of plaque and hence easily displaced with rinses and sprays. .
All individuals develop plaque and materia alba. Through regular brushing and flossing, these organized colonies of bacteria are disturbed and eliminated from the oral cavity. In general, the more effective one's brushing, flossing, and other oral homecare practices, the less plaque will accumulate on the teeth. However, if, after 24 hours in the oral environment, biofilm remains undisturbed by brushing or flossing, it begins to absorb the mineral content of saliva. Through this absorption of calcium and phosphorus from the saliva, oral biofilm transforms from the soft, easily removable plaque into a hard substance known as calculus. Commonly known as 'tartar', calculus provides a base for new layers of plaque biofilm to settle on and builds up over time.

CAVITY FILLING
Cavity filling is a way to restore a tooth which is damaged by decay back to its normal function and shape. In denta smile first we removes the decayed tooth material, cleans the affected area, and then fills the cleaned out cavity with a filling material.
Types of filling which we provide in denta smile
- COMPOSITE FILLING
- GIC FILLING
- CHANGING SILVER COLOURED FILLING TO TOOTH COLOURED FILLING

These are tooth coloured restorations available in various shades to provide natural look to the restored teeth. Made from a mixture of glass and quartz in resin, the composite filling requires less tooth cutting and is in accordance with minimal invasive dentistry. These are also hard wearing and compliment the adjoining teeth.
It is a dental restorative material used for filling teeth and as luting cement. There bond chemically to dental hard tissues and release fluoride for a relatively long period. They are tooth – colored and addition of resin has further improved their translucency but are still rather opaque and not as aesthetic as composite – resins. It is a bio-compatible material. It requires minimal cavity preparation hence easy to use on children
All individuals develop plaque and materia alba. Through regular brushing and flossing, these organized colonies of bacteria are disturbed and eliminated from the oral cavity. In general, the more effective one's brushing, flossing, and other oral homecare practices, the less plaque will accumulate on the teeth. However, if, after 24 hours in the oral environment, biofilm remains undisturbed by brushing or flossing, it begins to absorb the mineral content of saliva. Through this absorption of calcium and phosphorus from the saliva, oral biofilm transforms from the soft, easily removable plaque into a hard substance known as calculus. Commonly known as 'tartar', calculus provides a base for new layers of plaque biofilm to settle on and builds up over time.

In olden days, silver color dental fillings were used which was unaesthetic and had other disadvantages like recurrence of decay due to weak bonding between filling and tooth. Apart from the aesthetic concern the mercury content in the Silver Amalgam fillings is hazardous to health because of its potential to induce toxic and allergic reactions directly proportional to the mercury exposure. So ‘Mercury Free Dentistry’ is the need of the hour. Besides, Silver Amalgam Fillings can be easily replaced by White Fillings

Root canal therapy
It is a sequence of treatment for the infected pulp of a tooth it involves removal of infected pulp,cleaning and shaping of canal,and filling or sealing it with bio material(gutta-percha)..
- Severe toothache which is during chewing or during contact with any extreme hot or extreme cold temperature material which is usually tolerated by the mouth
- Darkening of the tooth
- Swelling seen in the areas of gums around the tooth
- When tooth is broken
Root canal treatment : A boon for the patients
In the past, when there was no existence of ‘Root canal treatment ‘ the only answer to extremely painful tooth or grossly destructed tooth was ‘Tooth removal!!!’ which is now the last resort when all the treatments have failed to save the tooth.So basically, root canal treatment is an advanced procedure to save a tooth in bad but restorable condition which was otherwise extracted and indicated for extraction. An untreated cavity is the most common cause of pulp infection. The decay erodes the enamel and dentin of the tooth until it reaches pulp and/or root canal. This allows bacteria to infect the pulp. The inflammation caused by the infection reduces the blood supply to the tooth and keeps it from healing. The second reason for a root canal treatment is damage to the pulp that can't be fixed. Trauma or a fractured tooth can damage the pulp. Sometimes, common dental procedures, such as preparing a tooth for a crown, end up hurting the pulp creating the need for a root canal. In certain cases, when the pulp is inflamed but not infected, it may heal on its own. Your dentist may want to see if this will happen before endodontic treatment. However, if the pulp remains inflamed, it can be painful and may lead to infection.
There are several steps in root canal treatment that your dentist will perform to save your tooth. You may have to make more than one visit.
- To begin with, the dentist will administer local anaesthesia to make sure that you will not experience pain during the procedure
- He will then isolate the tooth with a rubber dam, which is a thin sheet of latex rubber or plastic to keep the tooth dry and isolated.
- A cavity is prepared using a bur, in the crown of the tooth into the pulp chamber.
- The pulp or remaining tissue is then carefully removed from both the pulp chamber and the root canals.
- Each root canal is then cleaned and shaped to allow it to be filled.
- Medication may be placed in the pulp chamber and root canals to help eliminate bacteria.
- A temporary filling may be placed in the crown opening to prevent saliva from entering the chamber and root canals, or your dentist might immediately begin the next stage of filling the root canal.
- During the next stage of treatment, after placing the rubber dam, the dentist will remove the temporary filling (if one was placed during the previous visit). The root canals are usually filled with gutta-percha, a rubber-like material made from various tropical trees.
- In the final step, the temporary filling is removed and the tooth may be restored by a crown or a filling to strengthen and improve its appearance.
- The crown may be made of porcelain or metal alloy, and the filling may be made of many different materials.
- You might be prescribed antibiotics and other medication during the course of your treatment.
Type of Root Canal Treatment
- Single sitting
- Multiple sitting

WISDOM TOOTH REMOVAL OR IMPACTED TOOTH REMOVAL
In majority of cases, there will not be enough room in the jaw for a wisdom tooth or all wisdom teeth to fully emerge. This can lead to several complications. If the exit of the wisdom teeth is stalled at the halfway point (soft impaction), this can make brushing and flossing the wisdom teeth extremely difficult. Food and bacteria builds up between the wisdom teeth and its neighboring molars, and decay and gum infection are very likely to occur. Crowded wisdom teeth in the upper jaw have a tendency to lean sideways and grate against the cheek. These wisdom teeth usually cause ulceration and chewing problems. A further problem is wisdom teeth crowding- the pressure from wisdom teeth may also force the other teeth closer together, and interfere with the bite. Gum disease and cyst formations are also complications of impacted wisdom teeth. Very rarely, tumours may also form from the wisdom teeth. Pressure from the wisdom teeth can also cause toothache on the tooth next to it. Ulceration can also be caused by wisdom teeth. Upper wisdom teeth may push sideways out of the gum and cause ulcers inside of the cheek..



Even though impacted wisdom teeth are not visible in the mouth they can cause a number of problems. Commonly, patients will go to their dentist because of pain in the back of the jaws. Removal of the offending impacted tooth or teeth usually resolves the problem. The impacted wisdom tooth itself may be the source of the pain or there may be an infection associated it. Bacteria that are always present in the mouth, can work their way down under the gum tissue and cause a painful infection around the crown of the wisdom tooth even though you can’t see the tooth. People often mistake repeated soreness of the gum tissue overlying the wisdom teeth as an effort by the teeth to erupt. Unfortunately this is often a warning sign that trouble is brewing. If this situations goes untreated for an extended period of time (removal of the impacted tooth), the infection may become chronic and lead to destruction of bone around the impacted tooth (a condition known as periodontal disease). This bone destruction can extend around the other teeth in the back of the mouth and lead to future tooth loss. The same types of bacteria that are responsible for infections can also cause tooth decay or cavities on the roots of the other molar teeth. Just the constant pressure from the impacted wisdom tooth can lead to destruction of the tooth or teeth adjacent to it. Although the overall occurrence of cysts and tumors associated with the jaws is low, when they do occur it is most frequently around an impacted wisdom tooth. The orthodontist may request that wisdom teeth be removal prior to braces as they may interfere with straightening the other teeth. Finally, an impacted wisdom tooth in the lower jaw occupies space that is usually filled by bone. This creates an inherent area of weakness in the lower jaw which may render it more susceptible to fractures (broken jaw)..
As soon as it is determined that the wisdom teeth will become impacted, they should be removed. This can usually be determined by sixteen or seventeen years of age as the jaws have attained the majority of their adult size. Removal of impacted wisdom teeth in this age group has several distinct advantages. Toothache prompts patients to come to the dentist. However, wisdom teeth do not usually cause pain until damage has already been done! Wisdom teeth removal surgery is best performed sooner rather than later. Firstly, at this age the roots are seldom fully formed, even though the tooth has become impacted. If left in place, the tooth will not erupt into the mouth but the roots will continue to grow. Removing an impacted wisdom tooth before the roots are fully formed is easier and less traumatic for the patient. Also, at this stage of patient development the bone surrounding the impacted tooth is more pliable. Typically, patient’s having impacted wisdom teeth removed in their mid-teens heal more rapidly and have a shorter and less complicated post-operative recovery..
During a consultation involving x-rays or OPG (panoramic x-ray) and examination, the dental surgeon or the oral surgeon can determine which wisdom teeth or wisdom tooth will be, or are, functional, and which ones need to be removed. In many cases all four wisdom teeth will need to be removed. The wisdom teeth removal commonly involves an incision to open the gum, and sometimes a small portion of the bone may need to be removed to provide access for the wisdom teeth removal. The wisdom teeth may also need to be divided into segments so it can be removed safely and easily. Perfect wisdom teeth technique and a lot of experience is a must for these surgical procedures. The incision in the gum may then need to be closed with stitches..
Many orthodontists believe that developing wisdom teeth can cause the front teeth to become over crowded, and often recommend wisdom teeth removal before or immediately after orthodontic treatment.
Impacted wisdom teeth fall into several categories. Mesioangular impaction is the most common and means the wisdom tooth is angled forward, towards the front of the mouth. Vertical impaction means the tooth is angled backwards, towards the rear of the mouth. Horizontal impaction means fully 90 degrees forward. Most of the time wisdom teeth with distoangulation are the easiest to extract in the maxilla and the most difficult in the mandible. The wisdom teeth with mesioangulation are easier to remove in the mandible and more difficult in the maxilla.

Orthodontics
Orthodontic treatments works by using appliances, braces and aligners to move teeth that are crooked or that do not fit together right. By fixing these problems, orthodontics can Improve the appearance, biting position , chewing function and keep your mouth healthy.
Normally the orthodontic treatment is begun between the ages 10 and 14. This is when a child's head and mouth are still growing and teeth are easier to straighten, treatment duration will be 8 months to 16 months based upon the severity of the condition. Certain jaw growth problems can be handled simply in mixed dentition period, before the permanent teeth erupt – hence the treatment can begin at eth age of 6 ! But it’s can be done at any age – better late than never. In some children with mouthbreathing habits, thumb sucking – the habits can be broken with orthodontic appliances. .
Type of Orthodontic Treatment
- REMOVABLE
- FIXED METAL
- FIXED CERAMIC
- FIXED SELF LIGATING
- INVISIBLE LINGUAL
- INVISIBLE INVISALIGN

REMOVABLE

FIXED METAL

FIXED CERAMIC

FIXED SELF LIGATING

INVISIBLE LINGUAL

INVISIBLE INVISALIGN





